From Challenges to Comfort: Palliative Care for Dementia Patients
Practical ways palliative care makes life more comfortable for dementia patients, addressing their physical and emotional needs with care.
Practical ways palliative care makes life more comfortable for dementia patients, addressing their physical and emotional needs with care.

Dementia is an umbrella term that encompasses a range of cognitive impairments that interfere with daily life, affecting memory, thinking, and social skills. As this condition unfolds, it can often lead to profound changes not only for the individual diagnosed but also for their loved ones. Understanding dementia requires a nuanced perspective, one that moves beyond the clinical definitions and delves into the lived experiences of those affected.
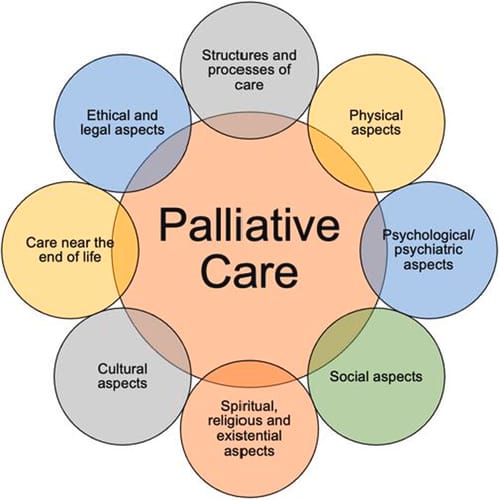
On the other hand, palliative care stands as a compassionate approach that prioritizes enhancing the quality of life for patients dealing with serious illnesses. Unlike curative treatment, which often focuses on fighting the disease itself, palliative care seeks to alleviate symptoms and stressors associated with the illness—fostering comfort and dignity through multifaceted support systems.
In the context of dementia, the integration of palliative care becomes vital. As dementia progresses, the person affected may experience not only physical challenges but also emotional and psychological distress. This is where the principles of palliative care can be instrumental in providing a holistic approach to treatment.
Dementia is characterized by a decline in cognitive function that can interfere with daily activities. Alzheimer’s disease is the most common form, but there are many others, including vascular dementia, Lewy body dementia, and frontotemporal dementia. Symptoms may vary widely, but often include memory loss, confusion, difficulty with language, and changes in mood and behavior.
As the disease progresses, one may lose the ability to communicate effectively, increasing frustration and isolation. Individuals with dementia may often find themselves grappling with lost connections—not just with others, but with their own sense of identity. Understanding these complexities is crucial for caregivers and healthcare providers alike. The emotional toll can be significant, as families navigate the shifting dynamics of their relationships, often requiring them to adapt to new ways of engaging with their loved ones. This emotional journey underscores the importance of support networks, education, and resources for caregivers, who play an essential role in the lives of those with dementia.
Palliative care emerges as a beacon of hope amidst the daunting landscape of dementia. Its role is not limited to managing physical symptoms; rather, it enfolds the individual—mind, body, and spirit. Through a team-based approach, palliative care specialists work alongside neurologists, geriatricians, and family caregivers to provide diverse avenues of support tailored to each individual's needs.
From managing pain and other distressing symptoms to offering guidance on navigating the healthcare system, palliative care encompasses every corner of the patient's journey. It's about creating a sanctuary where patients can share their fears and aspirations, all while their dignity remains intact. With empathy at its core, palliative care fosters connections that can alleviate the profound loneliness often experienced in advanced stages of dementia. Additionally, palliative care teams can assist families in making difficult decisions regarding treatment options and end-of-life care, ensuring that the wishes and values of the patient are honored. This collaborative approach not only enhances the quality of life for those with dementia but also provides crucial support for families as they face the emotional challenges of caregiving and the impending loss of their loved ones.
The intersection between dementia and palliative care is where the complexities of the human experience are most apparent. Individuals with dementia face a unique set of challenges that require tailored support—this is where the synergy of these two fields proves beneficial.
As dementia progresses, so too does the need for palliative interventions. The continual monitoring and proactive management of symptoms ensure that patients receive care that is both timely and compassionate. Recognizing the importance of dignity in the face of such a challenging diagnosis can empower individuals and families alike.
The need for palliative care in dementia is undeniable. Studies reveal that many people with advanced dementia experience physical pain, psychological distress, and existential fears that may go unaddressed in traditional healthcare settings. Integrating palliative care can counteract these issues, providing essential support that promotes a better quality of life.
Furthermore, families often need help navigating this labyrinthian journey. Many caregivers are thrust into their roles with little to no preparation; they may experience their own emotional burden, leading to stress and fatigue. The inclusion of palliative care in dementia management not only aids the patient but also serves as a lifeline for families, offering guidance and respite when they need it most. This support can take many forms, including counseling services that help families process their emotions, educational resources that clarify the stages of dementia, and respite care options that allow caregivers a much-needed break.

Palliative care does not replace standard dementia treatment; rather, it complements and enriches it. By focusing on symptom management and psychosocial support, it allows patients and families to engage more meaningfully with other therapies and day-to-day activities. These complementary services unite medical expertise with the emotional richness of shared human experience, ultimately crafting a multifaceted approach to care.
In addition, through regular assessments and personalized planning, caregivers and healthcare providers can ensure that evolving needs of the patient are met. It transforms care from a clinical mechanism into a holistic journey, where each step is taken in collaboration and respect. This collaborative approach fosters an environment where patients can express their preferences and wishes, ensuring that their voices are heard even as their cognitive abilities decline. Moreover, palliative care teams often include a diverse array of professionals—physicians, nurses, social workers, and chaplains—who work together to address the physical, emotional, and spiritual dimensions of care, creating a comprehensive support network for both patients and families alike.
Establishing an effective palliative care strategy for individuals with dementia requires a careful evaluation of their unique experiences. Various components merge to provide support across physical, emotional, and social dimensions.
One of the foremost roles of palliative care in dementia is the development of pain management strategies. Many individuals with later-stage dementia may not be able to articulate discomfort, making it essential to recognize non-verbal cues and behavioral changes. Management techniques may include:
Additionally, caregivers are encouraged to maintain a consistent routine, as familiarity can significantly reduce anxiety and discomfort for individuals with dementia. Incorporating sensory stimulation, such as aromatherapy or tactile activities, can also play a crucial role in alleviating pain and enhancing overall well-being. By adopting a holistic approach, palliative care teams can better address the multifaceted nature of pain in dementia patients, ensuring that their quality of life is prioritized.

The emotional and psychological support provided by palliative care is equally indispensable. With dwindling cognitive abilities, individuals may experience heightened levels of anxiety and depression. Psychologists and social workers can lend essential expertise, helping patients and families process these feelings and find coping strategies.
Support groups can serve as a sanctuary where caregivers can connect, share experiences, and alleviate feelings of isolation. Ultimately, fostering emotional well-being enables individuals and families to cultivate resilience in the face of adversity, allowing them to cherish moments together despite the challenges. Furthermore, incorporating mindfulness practices and relaxation techniques can empower both patients and caregivers, offering tools to navigate the emotional landscape of dementia. These practices not only enhance emotional regulation but also promote a sense of peace and acceptance in the midst of uncertainty.
Palliative care for dementia recognizes that the journey affects not just the patient but also their family and caregivers. Support services can include educational resources aimed at teaching families about the disease process, methods for effective communication, and strategies for self-care.
Moreover, respite care is a vital component, allowing caregivers to take necessary breaks without guilt. Acknowledging the emotional toll on caregivers is essential in creating a supportive environment where everyone can thrive during this challenging time. In addition to respite care, establishing a network of community resources can significantly ease the burden on families. Access to meal delivery services, transportation assistance, and home health aides can provide invaluable support, allowing caregivers to focus on their loved ones while ensuring their own needs are met. By fostering a collaborative approach, palliative care can enhance the overall experience for both patients and their families, creating a more compassionate and understanding atmosphere during this difficult journey.
Despite the myriad benefits of palliative care for those with dementia, significant challenges persist in its implementation. Understanding these obstacles helps illuminate paths for improvement.
One of the most profound challenges is communication. As dementia progresses, the ability to articulate needs and feelings diminishes, complicating the delivery of care. Healthcare providers must adopt empathetic approaches, utilizing non-verbal cues and other meaningful interactions to understand patient experiences fully.
Families also face difficulties in connecting with their loved ones, which can exacerbate feelings of helplessness. Training in effective non-verbal communication methods is vital for both caregivers and healthcare professionals, as it helps forge emotional connections even when words fail.
Ethical considerations loom large in the realm of dementia care. Questions surrounding autonomy and decision-making become particularly pertinent as individuals lose cognitive abilities. Who speaks for the patient when they can no longer voice their desires? What measures are in place to ensure that their wishes are honored? These dilemmas necessitate delicate handling, involving family discussions and advance care planning.
Palliative care providers must navigate these ethical waters with sensitivity and compassion, striking a balance between respecting the patient’s wishes while still ensuring their safety and comfort. People with dementia are especially vulnerable to being taken advantage of, phone scams, and even elder abuse. Engaging families in the decision-making process promotes alignment and respects the dignity of the individual.

The impact of palliative care on the quality of life for individuals with dementia is nothing short of transformative. By focusing on dignity and comfort, the complex web of challenges can begin to unwind in a supportive environment.
Palliative care's primary aim is to relieve suffering while enhancing comfort and dignity. With tailored pain management strategies, patients can experience reduced physical discomfort, allowing them to engage more meaningfully with their environment and loved ones. In turn, this leads to improved satisfaction in daily life.
Additionally, respecting individual preferences can empower patients, giving them a sense of agency even as their cognitive abilities decline. These small acknowledgements—choosing a favorite dish, selecting music to listen to—can significantly enhance their quality of life.
The emotional well-being of both patients and caregivers flourishes under comprehensive palliative care. By addressing mental health needs, providing support networks, and fostering connections, emotions can be navigated and expressed in a healthier manner. This supportive embrace breeds resilience during the most trying times.
Ultimately, the integration of palliative care within dementia treatment leads to a richer, fuller life where moments of joy coexist with challenges. It allows families to focus on celebrating life rather than solely coping with loss, creating memories that will resonate beyond the confines of illness.
As our understanding of dementia and palliative care evolves, so too does our ability to enhance the quality of life for those affected. Together, they create pathways toward compassion, understanding, and dignity—bathed in the shared humanity that defines us all.