From Challenges to Comfort: Palliative Care for Dementia Patients
Practical ways palliative care makes life more comfortable for dementia patients, addressing their physical and emotional needs with care.
Lewy Body Dementia doesn’t arrive neatly labeled; its symptoms mimic other conditions, from Alzheimer’s to Parkinson’s. But some clues are unique.

Lewy Body Dementia is a condition that arrives with little fanfare and a heap of complications, often disguised as something else entirely such as Alzheimer's disease. Identifying its symptoms early can make a world of difference in managing it effectively. Below, we’ll untangle the clues to help you recognize the signs that may point to this challenging diagnosis, as well as what to do about it.
One of the first hints of LBD may appear through the eyes—though not in the usual way. Visual hallucinations, often startlingly vivid, can emerge. These might involve lifelike images of people, animals, or objects that aren’t really there. Interestingly, such visions are more common with LBD than other types of dementia, affecting up to 80% of individuals. If someone mentions "seeing things" in a way that feels real but isn’t, it’s worth paying attention.
Cognitive fluctuations might sneak into daily life, with sharp changes in alertness or focus. One moment, the individual could seem entirely lucid, and the next, disoriented or inattentive. These swings are distinct and may occur not only from one day to the next but even within the same day. Unlike the slow decline typical of other dementias, LBD’s variability stands out.
Though movement changes may not dominate early on, small clues often make their debut:
These subtle alterations can provide important clues long before major mobility issues develop.
Sleep doesn’t remain restful for many with LBD. REM sleep behavior disorder—a rather dramatic-sounding name—manifests as physical actions during dreaming. This could involve yelling, kicking, or acting out imagined scenarios. For some, these disruptions happen years before any other symptoms appear, making sleep habits a surprising yet a very notable factor in early detection.

Cognitive symptoms, often overlooked in the early stages, may involve difficulty with spatial awareness (like judging distances), problem-solving, or even simple attention. Memory lapses, while present, might take a backseat compared to the prominence they have in Alzheimer’s.
Autonomic nervous system changes—those subtle shifts in bodily functions—can hint at LBD’s presence:
These signs, while not as obvious as cognitive or visual symptoms, add very significant pieces to the puzzle.
LBD often arrives with emotional baggage. Depression, anxiety, and even paranoia can appear, sometimes as early markers of the disease. Apathy may replace motivation, leading to confusion about whether the changes are psychological, physical, or both.
To recognize LBD’s shadow, focus on patterns and clusters of symptoms rather than isolated events. Repeated hallucinations, fluctuating cognition, or early movement changes can be enough reason to consult a professional. A neurologist familiar with LBD can assess these concerns more deeply.
Early identification doesn’t just clarify what’s happening—it opens doors for better management, planning, and support. When the symptoms feel overwhelming, understanding becomes the anchor that steadies the ship.
Managing a loved one's Lewy Body Dementia (LBD) demands a nuanced approach, one that balances medical expertise with compassionate care. Dr. Mehrdad Yadi stresses that proper management starts with the involvement of specialists—neurologists, geriatricians, and psychiatrists—who are experienced in the complexities of this condition.
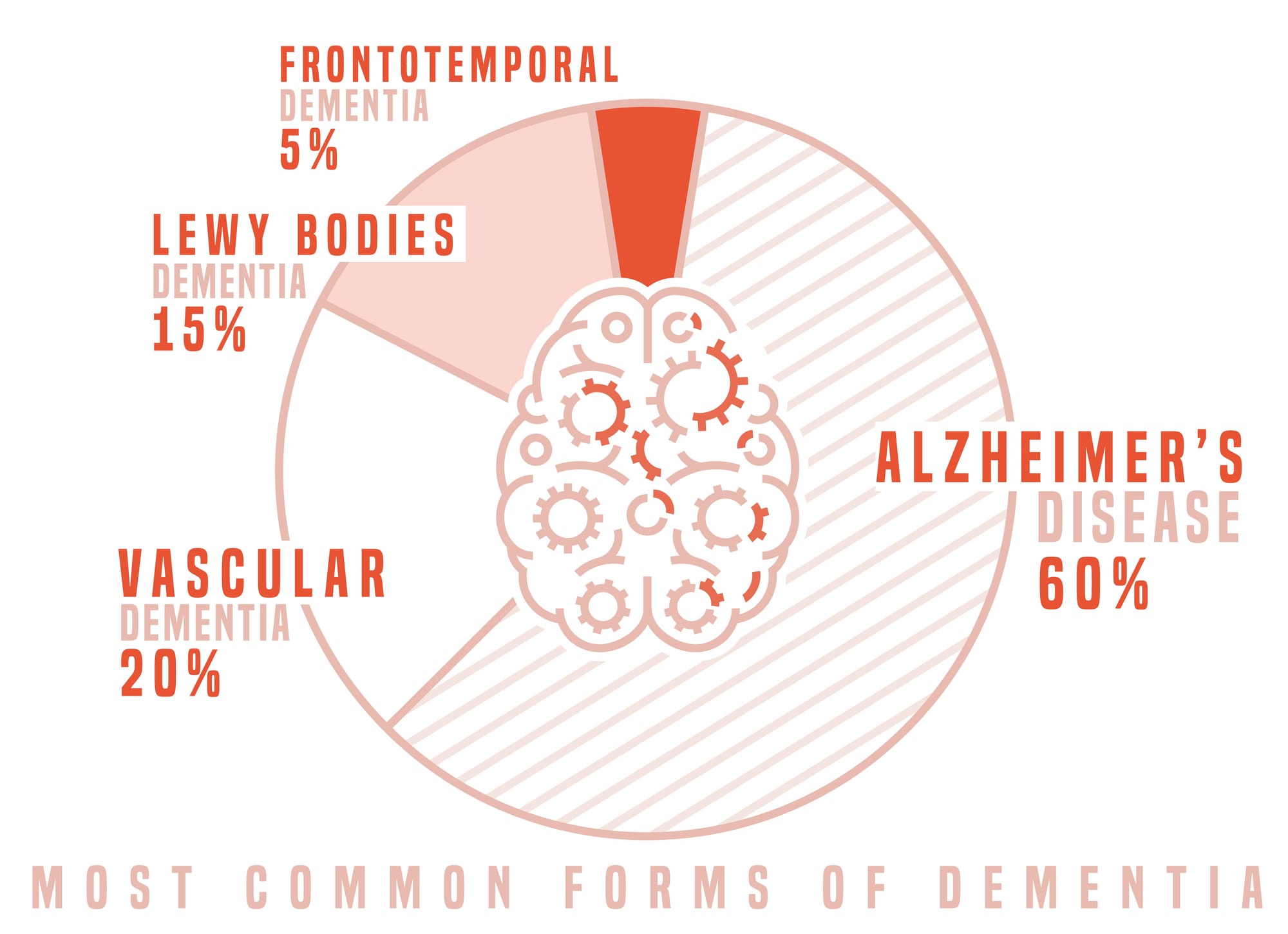
LBD’s symptoms often overlap with other dementias, making accurate diagnosis tricky. Specialists familiar with LBD can distinguish its unique features, such as cognitive fluctuations, visual hallucinations, and sensitivity to medications, ensuring patients receive appropriate care. Misdiagnosis or generic treatments may exacerbate symptoms, particularly when medications like antipsychotics are prescribed without caution.
Caregivers play a very important role in daily management, often navigating fluctuating symptoms and ensuring a safe environment. Resources like the Alzheimer’s Association and the American Geriatrics Society, which provide guidance, education, and support networks to families coping with LBD.