From Challenges to Comfort: Palliative Care for Dementia Patients
Practical ways palliative care makes life more comfortable for dementia patients, addressing their physical and emotional needs with care.
Palliative care focuses on providing comfort, easing symptoms, and improving quality of life for those facing serious, long-term illnesses. Unlike traditional care, which often aims to cure, palliative care addresses the whole person—including physical, emotional, and social needs.

As dementia and Alzheimer’s progress, they bring profound changes that extend beyond memory loss, often affecting mood, behavior, and physical health in ways that can be deeply challenging for both patients and families. Palliative care is a compassionate approach that steps in to address these very changes, focusing on comfort, dignity, and quality of life. For those with dementia or Alzheimer’s, palliative care offers personalized care that respects each person’s experiences, values, and needs, while also providing crucial support to their families.
Let’s take a closer look at how palliative care for dementia and Alzheimer’s patients helps manage symptoms, supports caregivers, and offers comfort throughout the journey.
Palliative care is fundamentally patient-centered, focusing on managing symptoms and improving comfort rather than curing the underlying disease. This approach seeks to enhance the patient’s quality of life by addressing a range of symptoms—such as pain, nausea, fatigue, and shortness of breath—and aims to ease psychological, emotional, and social stressors that often accompany chronic illness. Palliative care practitioners work to create a calm, supportive environment that enables patients to feel more comfortable both physically and mentally. For instance, a patient with advanced cancer may receive medication specifically to manage pain or nausea and support to alleviate anxiety or depression.
In contrast, traditional or “normal” care is often disease-focused and aims primarily at diagnosing and treating conditions with the goal of achieving a cure or managing the illness to restore health. For example, a patient diagnosed with pneumonia may undergo a series of tests to confirm the type of infection and be prescribed antibiotics to eradicate it, with follow-up visits to ensure a full recovery. Normal care is frequently goal-oriented, with a focus on measurable improvements, such as symptom reduction, physical healing, and overall recovery.
Palliative care is about caring for the person, not just managing symptoms. For patients with dementia, this means prioritizing comfort, well-being, and quality of life over invasive treatments. This approach is especially beneficial for dementia and Alzheimer’s, which gradually limit a person’s ability to communicate, remember, and make decisions. While the aim is not to cure these illnesses, palliative care is focused on easing physical and emotional discomfort, adapting to the patient’s evolving needs, and giving families the tools to support their loved ones with compassion and understanding.
Palliative care for dementia is built on a foundation of respect for the individual’s needs, beliefs, and preferences. This approach involves:
Complete Care
Palliative care looks beyond physical needs, addressing the full spectrum of emotional, social, and spiritual well-being. For dementia patients, this holistic approach means creating spaces that bring comfort, incorporating familiar objects or soothing sounds to reduce anxiety. It’s about connecting with the patient on multiple levels, helping them feel a sense of calm and belonging even when memory fades.
Patient-Centered Care
Every care plan is tailored to the individual, honoring their personal values, preferences, and past experiences. This approach respects each person’s routines and unique personality, even as communication becomes limited. Caregivers learn to follow the patient’s cues, keeping familiar comforts and routines that bring peace, ensuring that care remains a true reflection of who the person is.
Family Involvement
Family members are necessary partners in palliative care, guiding decisions and daily routines based on what they know best about their loved one. The care team offers tools and support to help families manage both practical and emotional challenges, recognizing the essential role they play. By equipping families with resources and guidance, palliative care strengthens the caregiving experience, helping everyone involved feel supported and prepared.

Palliative care offers strategies for managing the range of symptoms dementia patients experience, from physical discomfort to behavioral changes. Effective symptom management enhances quality of life for both the patient and their caregivers.
Physical Symptoms: Dementia patients may experience pain, sleep disturbances, and mobility issues. Palliative care providers use gentle, non-invasive treatments—such as warm baths, massage, and sometimes low-dose medications—to ease these symptoms without overwhelming the patient. Maintaining a comfortable environment with minimal noise and sufficient lighting can further reduce discomfort.
Behavioral and Psychological Symptoms: Dementia can bring about anxiety, depression, confusion, and even aggression. Non-drug approaches, like music therapy, aromatherapy, and structured daily routines, can help reduce these symptoms. Palliative teams work closely with families to find activities and strategies that engage the patient’s attention and soothe their emotions.
End-of-Life Considerations: Advanced dementia brings its own challenges, including difficulty swallowing and increased vulnerability to infections. Palliative care teams help families prepare for these stages, providing guidance on feeding adjustments, hydration, and recognizing when comfort measures may be more appropriate than aggressive treatments.
Caregivers of dementia patients face a unique set of challenges, often juggling daily care with the emotional strain of seeing a loved one change. Palliative care prioritizes caregiver support, offering education, resources, and a compassionate ear.
Education on Disease Progression: Families are given realistic information about what to expect as dementia advances. Understanding potential changes in behavior, memory, and physical function helps families anticipate and respond compassionately to their loved one’s needs.
Emotional Support: Caregiving can be exhausting, and the emotional toll can lead to stress, anxiety, and even burnout. Palliative care teams often offer counseling for both families and patients, support groups, and respite care options to help caregivers sustain their own well-being.
Advanced Directives and Care Planning: Palliative care encourages families to have conversations about their loved one’s wishes early on. Care plans are established to honor the patient’s preferences, ensuring that decisions about treatments and interventions align with their values.
As dementia progresses, care often transitions across settings—from home to assisted living facilities or hospice. Palliative care provides continuity, ensuring that patients receive compassionate, consistent support no matter where they are.
Home Care and Hospice: Palliative care helps families arrange in-home services or hospice when the time comes, supporting patients with comfort measures that allow them to stay at home whenever possible. Hospice often becomes the natural next step, offering further support as patients reach the end-of-life stage.
Community Resources: Finding resources in the community, such as support groups, senior centers, and respite programs, can relieve the burden on families and improve the patient’s quality of life. Palliative teams often assist families in locating these services.
Collaborative Team Approach: Palliative care brings together a team of professionals, including doctors, nurses, social workers, and counselors, who work together to support the patient and family. This team approach ensures that every aspect of care, from medical to emotional, is covered.
Introducing palliative care early in a dementia diagnosis can bring significant benefits. When patients and families engage with palliative services early, they’re better prepared for the future and can take full advantage of the care available.
Enhanced Quality of Life: By addressing symptoms and supporting mental well-being, palliative care reduces hospitalizations and the need for aggressive treatments, helping patients live more comfortably.
Family Satisfaction: Early palliative involvement often leads to better patient and family experiences, as they receive guidance and support from the beginning. This support fosters a sense of control and reassurance during a challenging time.
Financial Considerations: Palliative care can reduce medical expenses by minimizing hospital visits and invasive procedures. This approach frees families to focus resources on comfort, support, and quality of life.

Palliative care is frequently misunderstood, especially in the context of dementia. Addressing these misconceptions can empower families to seek the support they need without fear or stigma.
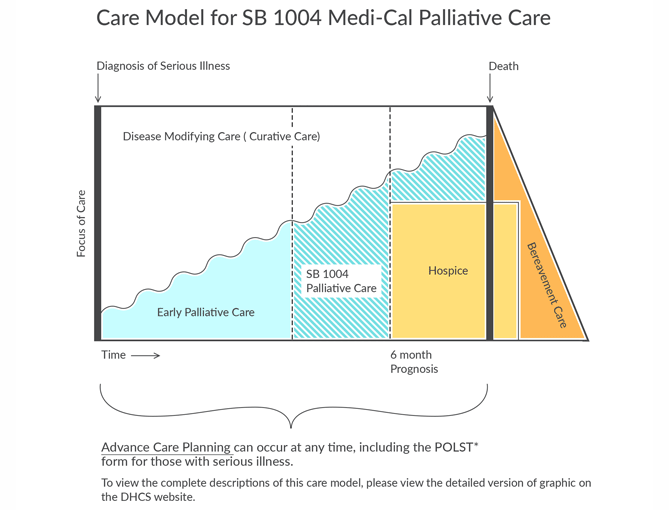
Palliative Care Isn’t Only for End of Life: Unlike hospice, palliative care can begin at any stage of illness, focusing on improving quality of life rather than "curing" a disease at any cost to the patient.
It Doesn’t Mean “Giving Up”: Many people worry that opting for palliative care means they’re “giving up” on their loved one. In reality, palliative care emphasizes comfort and dignity, creating space for patients to live as fully as possible within their abilities.
Family Empowerment: Palliative care provides families with options and information, allowing them to make informed decisions that align with their loved one’s wishes. It is a support, not a replacement, for family involvement in the caregiving process.
Palliative care for dementia and Alzheimer’s patients is about finding a pathway through the challenges of illness with grace and compassion. It provides a steady hand for families navigating an unfamiliar path, helping both patients and caregivers feel respected, understood, and cared for. By focusing on comfort, dignity, and individualized support, palliative care opens a door to a more peaceful experience, ensuring that both the patient and their loved ones find the support they need to face this journey together.