From Challenges to Comfort: Palliative Care for Dementia Patients
Practical ways palliative care makes life more comfortable for dementia patients, addressing their physical and emotional needs with care.
Hypertension affects nearly 90% of adults by age 80, yet managing it requires more than medication. Discover the causes, challenges, and practical strategies to keep blood pressure in check while balancing the unique needs of older adults.

Hypertension, or high blood pressure, is one of the number one conditions in the United States that leads directly to death. It often creeps in without warning, causing no obvious symptoms until real damage has been done. For older adults, the stakes are especially high—hypertension doesn’t just increase with age; it practically feels inevitable.
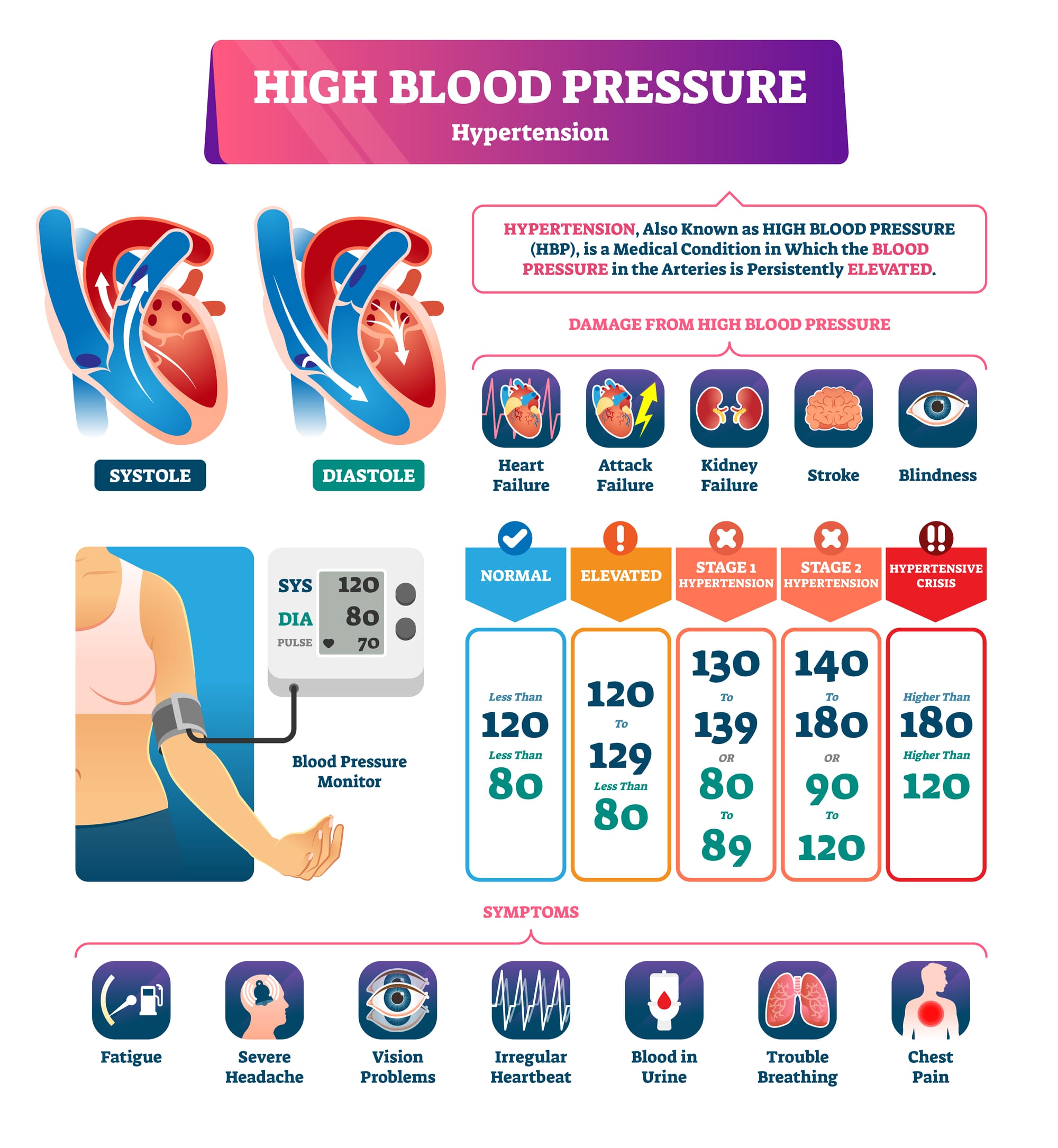
Unchecked over a long period of time, high blood pressure strains the heart, harms the kidneys, and dramatically raises the risk of a stroke. Managing it takes more than pills; it requires understanding how aging changes the body and adjusting the approach to fit each person’s unique needs.
High blood pressure is extremely widespread among older adults. The statistics highlight how it becomes almost inevitable with age:
These numbers aren’t just statistics—they reflect how aging increases the strain on the heart and blood vessels. Recognizing how common hypertension is in older adults shows the importance of regular check-ups and early treatment.

Hypertension doesn’t appear out of nowhere. It’s shaped by a mix of biology and lifestyle. Unfortunately, more than one of these complications can happen simultaneously, making the management of hypertension especially tricky. Here’s what’s working against us as we age:
When we’re young, our arteries are flexible and elastic, expanding with each heartbeat to let blood flow smoothly. Over time, these pathways stiffen. Blood struggles to move, and the heart pumps harder to compensate. This extra effort raises systolic pressure (the top number in a blood pressure reading).
Many older adults become less active as life slows down, and extra weight can sneak on. Every additional pound adds to the workload on the heart, making blood pressure rise. But here’s the good news: even light exercise—like a daily walk or some gardening—can help bring those numbers down.
Salt is everywhere, and it’s hard to tell how prevalent it is in some consumer packaged goods. From canned soups to frozen dinners, processed foods are loaded with sodium, which makes the body retain water. That extra fluid increases blood pressure. Cutting back on processed foods and seasoning meals with herbs instead of salt can help keep sodium levels in check.
Diabetes, kidney disease, and other health issues complicate the picture. These conditions force the heart and blood vessels to work overtime, creating a vicious cycle where each condition contributes to making the others worse. Treating underlying problems quickly is key to controlling blood pressure and your overall health.
Sometimes, high blood pressure is simply in your genetic cards. New research on lipids and genetic testing can let you know what is happening with your blood pressure risk. While you can’t rewrite your genes, you can manage the risk with regular checkups, a heart-healthy diet, and staying active.

For older adults, diagnosing hypertension accurately isn’t as simple as using a blood pressure cuff one time in the doctor’s office. Your blood pressure can wildly fluctuate for various reasons, making it necessary to monitor your blood pressure at home, sometimes multiple times a day.
White coat hypertension is an intuitively odd, but common phenomenon where your blood pressure reads higher in a doctor's office than it does in your everyday life. It’s named for the white coats traditionally worn by doctors and nurses, which can symbolize the stress or anxiety some people feel during their medical appointments. While it may seem harmless and simple, this condition can truly complicate diagnosis and your management of hypertension.
For some people, stepping into a doctor’s office triggers a barely noticeable fight-or-flight response. It’s not always just about fear of the doctor—it can be the tension of being examined, the coldness of the table, or even underlying anxiety about upcoming health news in general. This stress activates the body’s nervous system, which:
The result is a reading that doesn’t reflect your usual blood pressure levels at home or during normal activities.
White coat hypertension isn’t rare, especially among older adults. Studies suggest it affects 15-30% of patients, though the exact numbers vary depending on age, gender, and individual anxiety levels. Interestingly enough, it’s more prevalent in individuals newly diagnosed with hypertension, which can further complicate diagnosis.
At first glance, white coat hypertension might seem like a small inconvenience. After all, if the blood pressure normalizes outside the clinic, what’s the harm? But the implications go deeper:
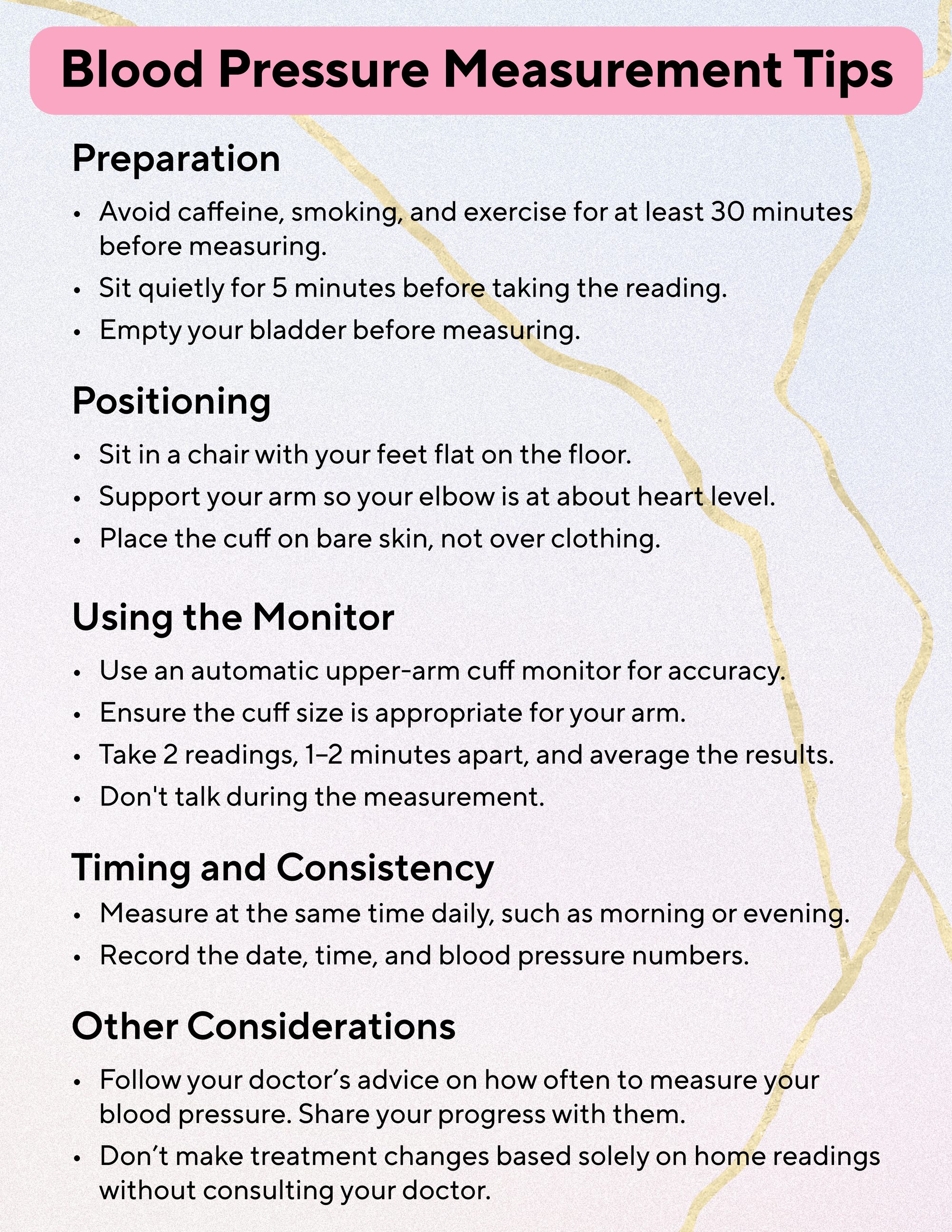
The best course of action is to regularly check your own blood pressure at home with your own monitor. Sit with your preferred arm raised at about the same level as your heart, ideally resting on a comfortable pillow. Don't cross your legs, and try to relax and sit calmly for one minute before taking the reading. Blood pressure rises with exercise and changes in movement, so if you've been downstairs all day and suddenly go upstairs to check your blood pressure, it is very possible that you can impact the reading.
Deciding how low to aim with blood pressure isn’t straightforward. Some experts recommend a target of less than 130/80 mmHg for people in their late 60s and 70s, as long as they can tolerate it. For those in their 80s and beyond, a slightly higher range—130-139/70-79 mmHg—might make more sense. Why the difference? Older adults often have other health issues, and pushing blood pressure too low can sometimes do more harm than good. The key is tailoring the goal to the individual, not just the chart.
You don’t have to overhaul your life to manage high blood pressure. Small, consistent changes can go a long way:
Doctors usually start with a cautious approach, starting with low doses to avoid side effects like dizziness or fatigue, as these can be especially concerning and dangerous for older adults. After discovering what can be tolerated well, they monitor how well the treatment is working and adjust as needed. It’s not just about lowering blood pressure; it’s about doing so in a way that minimizes risks and improves overall well-being.
It is important to make sure that you talk with your doctor about each of your medications. All medications work in different ways, and the choices depends on factors like kidney health, heart function, and other medical conditions. However, some medications don't work for everyone and sometimes you have to make suboptimal decisions about how to proceed. A great example is if you have kidney disease and high blood pressure, sometimes the available options can be very limited.
Here are the most common options:
Choosing a medication is as much about the patient as it is about the condition. For instance:
This tailored approach ensures that treatment doesn’t just lower blood pressure but also fits into the patient’s daily life without adding unnecessary complications.
Managing hypertension in older adults isn’t just about hitting target numbers—it’s about balancing treatment with the realities of aging. The goal is to reduce risks while maintaining quality of life, mobility, and independence. This requires a thoughtful approach that considers the unique challenges older adults face.
For older adults who are frail, aggressive blood pressure treatment can do more harm than good. Lowering blood pressure too quickly or too much can lead to fatigue, weakness, and even falls—serious risks for this group. In these cases, doctors often prioritize keeping patients mobile and maintaining their overall quality of life over strict adherence to blood pressure targets.
There’s a strong link between high blood pressure and cognitive decline. Uncontrolled hypertension can damage the brain’s small blood vessels, increasing the risk of dementia. Managing blood pressure thoughtfully can help preserve memory and mental sharpness, giving older adults a better chance of staying independent as they age.
Older adults are more prone to dizziness, especially when standing up too quickly—a condition called orthostatic hypotension. Rapid or excessive blood pressure reduction can make this worse, increasing the likelihood of dangerous falls. To avoid this, doctors aim for gradual adjustments in blood pressure and regularly check how treatment affects balance and stability.